Medical microbiology and virology (doctor)
Microbiologists and virologists diagnose, treat and prevent the spread of infection, making a major contribution to clinical infection management.
Both roles demand excellent clinical skills as well as first-class laboratory knowledge.
Life as a microbiologist
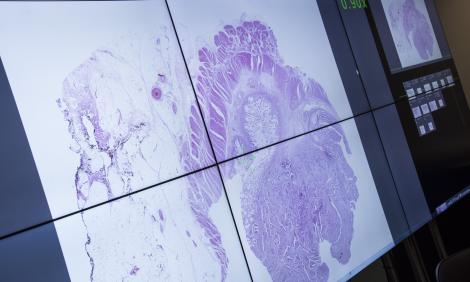
You’ll provide advice on the likely causes and suggest the best test to diagnose a patient suspected of having an infectious disease. The testing you’ll do may involve the identification of parasites under a microscope, the use of biochemical tests to identify colonies of bacteria or the use of molecular tests to identify organisms (or even specific genes), which may govern an organism’s behaviour.
You’ll be expected to interpret tests results and recommend appropriate further investigation and antibiotic treatment.
It’ll be your responsibility to ensure the delivery of prompt and accurate test results for patients. In cases where antimicrobial drugs are required, you’ll provide advice concerning the choice of such drugs and the duration of treatment.
The side effects of treatment along with the potential risk of encouraging further infections (some of which may be antibiotic-resistant) must be considered in tandem with any medical problems or allergies the patient might have. In doing so, you’ll play a major role in controlling the spread of infectious diseases, including the spread of hospital-based ‘super-bugs’ such as MRSA.
In your role, you’ll also contribute to the protection of public health by monitoring the patterns of infectious diseases.
You’ll usually work with clinical colleagues, GPs and laboratory staff rather than with patients directly. You’ll be hands-on and expected to perform:
- traditional culture techniques such as microbiological stains
- measuring antibody response to infection
- detection of microbial antigens
- nucleic acid amplification (polymerase chain reaction)
Life as a virologist
Your role will focus on viral infections, and your time will be divided between laboratories and clinics as well as working on hospital wards and in the wider community.
You’ll manage HIV/AIDS and other blood-borne infections such as hepatitis B and C. But the role of a virologist is rapidly evolving, and increasingly your challenge will be to manage the spread of emerging viruses like Covid-19 and combat the threat from bioterrorism and the use of agents like smallpox.
You’ll usually work directly with clinical colleagues, GPs and laboratory staff rather than with patients directly. You’ll be hands-on and expected to perform:
- antigen detection techniques
- high-throughput nucleic acid extraction techniques
How much can I earn?
You’ll first earn a salary when you start your foundation training after medical school. Find out details of current salary ranges for foundation and specialty training, SAS doctors and consultants on the 'Pay for doctors' page.
How about the benefits?
- make a difference
- flexible and part-time working
- high income early in your career
- work anywhere in the world
- excellent pension scheme
- good holiday entitlement
- NHS discounts in shops and restaurants
Must-have skills
- excellent communication skills to manage a wide range of relationships with colleagues, and patients and their families
- emotional resilience, a calm temperament and the ability to work well under pressure
- teamwork and the capacity to lead multidisciplinary teams
- problem-solving and diagnostic skills
- outstanding organisational ability and effective decision-making skills
- first-class time and resource management for the benefit of patients
Entry requirements
Your first step is medical school. Typically, you’ll need excellent GCSEs and three A or A* passes at A level including chemistry for a five-year undergraduate degree in medicine. Many medical schools also ask for biology and others may require maths or physics.
If you already have a degree, you could study for a four-year postgraduate degree in medicine.
You’ll need to pass an interview and admissions test. You’ll be asked to show how you demonstrate the NHS values such as compassion and respect.
Some medical schools look to recruit a mix of students from different backgrounds and geographical areas, so your educational and economic background and family circumstances could be considered as part of your application.
"I’m passionate about my job because I believe in the importance of what I’m doing – promoting the rational use of antibiotics and of diagnostic tests. I love the breadth and variety that the specialty provides, and the fact that I’m learning new things every day."
Read Jonathan's story.
What are my chances of starting a career as a microbiologist or virologist?
There are approximately 444 microbiologist and 11 virologists working in the NHS in England.
How to become a microbiologist or virologist
After medical school, you’ll join the paid two-year foundation programme where you’ll work in six placements in different settings.
After your foundation programme, you can apply for paid specialty training to become a microbiologist or virologist, which will take a minimum of four years.
You may be able to train part time, for example for health reasons or if you have family or caring responsibilities.
Where a career as a microbiologist or virologist can take you
There are no sub-specialties in microbiology and virology but there are many opportunities to undertake research.
-
Consultant - Infection / Microbiology / Virology
Truro, TR1 3LJ
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- Royal Cornwall Hospitals Trust
-
Specialist Doctor in Medical Microbiology
Carlisle, CA2 7HY
- Salary :
- £100870.00 to £111441.00
- Type :
- Fixed-Term
- Employer :
- North Cumbria Integrated Care NHS Foundation Trust
-
ENT Doctor
Swindon, SN3 3RB
- Salary :
- £550.00
- Type :
- Bank
- Employer :
- CHEC
-
Specialty Doctor
London, W6 8NF
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- West London NHS Trust
-
Specialty Doctor
Bolton, BL4 0JR
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- Bolton NHS Foundation Trust
-
Dermatology Doctor
Swindon, SN3 3RB
- Salary :
- £550.00
- Type :
- Bank
- Employer :
- CHEC
-
ENT Doctor
Canterbury, CT1 1BN
- Salary :
- £550.00
- Type :
- Bank
- Employer :
- CHEC
-
Specialty Doctor
Stockton-on-tees, TS18 1DN
- Salary :
- £90317.14 to £101316.49
- Type :
- Permanent
- Employer :
- Change Grow Live
-
Dermatology Doctor
Canterbury, CT1 1BN
- Salary :
- £550.00
- Type :
- Bank
- Employer :
- CHEC
-
Dermatology Doctor
Canterbury, CT1 1BN
- Salary :
- £550.00
- Type :
- Bank
- Employer :
- CHEC
-
Specialty Doctor
London, SE5 8UH
- Salary :
- £59175.00 to £95400.00
- Type :
- Permanent
- Employer :
- Guy's and St Thomas' NHS Foundation Trust
-
Dermatology Doctor
Worthing, BN11 3BN
- Salary :
- £550.00
- Type :
- Bank
- Employer :
- CHEC
-
ENT Doctor
Worthing, BN11 3BN
- Salary :
- £550.00
- Type :
- Bank
- Employer :
- CHEC
-
Specialty Doctor
London, NW3 2QG
- Salary :
- £61542.00 to £99216.00
- Type :
- Fixed-Term
- Employer :
- Royal Free London NHS Foundation Trust
-
Specialty Doctor Orthodontics
Wrexham, LL13 7TD
- Salary :
- £62117.00 to £99216.00
- Type :
- Permanent
- Employer :
- Betsi Cadwaladr University Health Board
-
Research Doctor (CRDC)
Truro, TR1 3HD
- Salary :
- £52656.00
- Type :
- Fixed-Term
- Employer :
- Royal Cornwall Hospitals Trust
-
Specialty Doctor - Breast
Southend / Broomfield, SS0 0RY
- Salary :
- £61542.00 to £99216.00
- Type :
- Fixed-Term
- Employer :
- Mid and South Essex NHS Foundation Trust
-
Specialty Doctor Ophthalmology
Hereford, HR1 2ER
- Salary :
- £61542.00 to £99216.00
- Type :
- Fixed-Term
- Employer :
- Wye Valley NHS Trust
-
Dermatology Specialty Doctor
Lincoln, LN2 5QY
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- United Lincolnshire Hospitals NHS Trust
-
Specialty Doctor - Dermatology
Basildon, SS16 5NL
- Salary :
- £61542.00
- Type :
- Fixed-Term
- Employer :
- Mid and South Essex NHS Foundation Trust
-
UTC Speciality Doctor
Hillingdon, UB8 3NN
- Salary :
- £61542.00 to £99216.00
- Type :
- Fixed-Term
- Employer :
- The Hillingdon Hospital NHS Foundation Trust
-
ST3 + Doctor Gastroenterology
Hereford, HR1 2ER
- Salary :
- £65048.00
- Type :
- Fixed-Term
- Employer :
- Wye Valley NHS Trust
-
Specialty Doctor - Oncology
Birmingham, B15 2TH
- Salary :
- £59175.00 to £95400.00
- Type :
- Fixed-Term
- Employer :
- University Hospitals Birmingham NHS Foundation Trust
-
Psychiatry Specialty Doctor
Leeds, LS12 2LB
- Salary :
- £70901.00 to £99216.00
- Type :
- Permanent
- Employer :
- Leeds and York Partnership NHS Foundation Trust
-
Speciality Doctor - Urology
Chesterfield, S44 5BL
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- Chesterfield Royal Hospital NHS Foundation Trust
-
Speciality Doctor Stroke
Eastbourne, BN21 2UD
- Salary :
- £49909.00 to £61825.00
- Type :
- Fixed-Term
- Employer :
- East Sussex Healthcare NHS Trust
-
Specialty Doctor / GPSI
Torquay, TQ2 7AA
- Salary :
- £61542.00 to £99216.00
- Type :
- Fixed-Term
- Employer :
- Torbay and South Devon NHS Foundation Trust
-
Medical Research Doctor
Cambridge, CB24 3BA
- Salary :
- £45000.00 to £60000.00
- Type :
- Permanent
- Employer :
- Optimum Patient Care
-
Trust Research Doctor
Barnstaple, EX31 4JB
- Salary :
- £65048.00 to £65048.00
- Type :
- Fixed-Term
- Employer :
- Royal Devon University Healthcare NHS Foundation Trust
-
Specialty Doctor - Radiology
London, N18 1QX
- Salary :
- £61542.00 to £99216.00
- Type :
- Fixed-Term
- Employer :
- Royal Free London NHS Foundation Trust
-
Urology Locally Employed Doctor
London, N18 1QX
- Salary :
- £52656.00
- Type :
- Permanent
- Employer :
- Royal Free London NHS Foundation Trust
-
Bank - Speciality Doctor - Anaesthetics
Essex, SS0 0RY
- Salary :
- Negotiable
- Type :
- Bank
- Employer :
- Mid and South Essex NHS Foundation Trust
-
Bank - Speciality Doctor - Urology
Essex, SS0 0RY
- Salary :
- Negotiable
- Type :
- Bank
- Employer :
- Mid and South Essex NHS Foundation Trust
-
Sexual Health Trust Doctor
Oxford, OX3 7LE
- Salary :
- £52656.00 to £73992.00
- Type :
- Fixed-Term
- Employer :
- Oxford University Hospitals NHS Foundation Trust
-
Specialty Doctor in Ophthalmology
Worcester, WR4 9FA
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- New Medical Systems Ltd
-
Specialist Doctor in Ophthalmology
Chesterfield, S44 5BL
- Salary :
- £100870.00 to £111441.00
- Type :
- Permanent
- Employer :
- Chesterfield Royal Hospital NHS Foundation Trust
-
Speciality Doctor/Clinical Fellow
Wolverhampton, WV3 9DH
- Salary :
- £52656.00 to £61542.00
- Type :
- Permanent
- Employer :
- Compton Care
-
Specialty Doctor -Forensic Psychiatry
London, W12 0AE
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- North London NHS Foundation Trust
-
Specialty Doctor - Stroke Medicine
Torquay, TQ2 7AA
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- Torbay and South Devon NHS Foundation Trust
-
Specialty Doctor (Part-time)
Dundee, DD5 1PL
- Salary :
- £59500.00
- Type :
- Permanent
- Employer :
- Cygnet Health Care
-
Specialty Doctor in Dermatology
Northampton, NN1 5BD
- Salary :
- £59175.00 to £95400.00
- Type :
- Permanent
- Employer :
- Northampton General Hospital
-
Bank Specialty Doctor/ GP
Chippenham, SN15 2AJ
- Salary :
- £70.00 to £80.00
- Type :
- Bank
- Employer :
- HCRG Care Group
-
Specialty Doctor - Cavendish House
Hastings, TN343AD
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- Sussex Partnership NHS Foundation Trust
-
Medical Retina Specialty Doctor
London, EC2V 1PD
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- Moorfields Eye Hospital NHS Foundation Trust
-
Trust Doctor in Anaesthetics
London, E11 1NR
- Salary :
- £44170.00 to £67610.00
- Type :
- Fixed-Term
- Employer :
- Barts Health NHS Trust
-
Specialty Doctor in Anaesthetics
Rotherham, S60 2UD
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- The Rotherham NHS Foundation Trust
-
Specialty Doctor in Dermatology
Bradford, BD5 0NA
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- Bradford Teaching Hospitals NHS Foundation Trust
-
Speciality Doctor in Dermatology
Harlow, CM20 1QX
- Salary :
- £61542.00 to £99216.00
- Type :
- Fixed-Term
- Employer :
- The Princess Alexandra Hospital NHS Trust
-
Named Doctor Safeguarding Children
Southall, UB2 4SD
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- West London NHS Trust
-
Speciality Doctor - West IMHT
Cannock, WS11 1JN
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- Midlands Partnership NHS Foundation Trust
-
Specialty Doctor in Psychiatry
St Helens, WA9 3DE
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- Mersey Care NHS Foundation Trust
-
Specialty Doctor - Male Acute
Harrow, HA1 3JL
- Salary :
- £80000.00 to £85000.00
- Type :
- Permanent
- Employer :
- Cygnet Health Care
-
Specialty Doctor - Palliative Medicine
Dorchester, DT1 2SL
- Salary :
- Negotiable
- Type :
- Permanent
- Employer :
- Weldmar Hospicecare
-
Bank - Speciality Doctor - Neurology
Essex, SS0 0RY
- Salary :
- Negotiable
- Type :
- Bank
- Employer :
- Mid and South Essex NHS Foundation Trust
-
Specialty Doctor - Emergency Department
Grimsby/Scunthorpe, DN15 7BH
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- Northern Lincolnshire and Goole NHS Foundation Trust
-
Specialty Doctor - Emergency Department
Steeton, BD20 6TD
- Salary :
- £61542.00 to £99216.00
- Type :
- Permanent
- Employer :
- Airedale NHS Foundation Trust
-
Treatment Doctor / Surgeon - 15 hours
Birmingham, B30 1DB
- Salary :
- £101000.00 to £151000.00
- Type :
- Permanent
- Employer :
- British Pregnancy Advisory Service (BPAS)
-
Specialty Doctor at Westminster CAMHS
London, W9 2NW
- Salary :
- £59175.00 to £95400.00
- Type :
- Permanent
- Employer :
- Central and North West London NHS Foundation Trust
-
Specialty Doctor in Palliative Medicine
PRESCOT, L34 2QT
- Salary :
- Negotiable
- Type :
- Permanent
- Employer :
- WILLOWBROOK HOSPICE
Showing 6 of 59 results
-
These organisations have further information about being a microbiology and virology doctor, particularly as your career progresses. Take a look.
European Society of Clinical Microbiology and Infectious Diseases