Clinical oncology
A clinical oncologist is a doctor who uses chemotherapy, radiotherapy and a range of other treatments to care for patients with cancer.
You’ll treat patients with all types of cancer using a combination of chemotherapy and radiotherapy, which separates the role from medical oncologists who use non-radiological treatments.
Life as a clinical oncologist
Your patient’s cancer diagnosis will be given by another specialist and your role will be to determine the type of treatment, which will require you to draw on your training and experience daily.
You’ll need to be prepared to answer all your patient’s questions about their condition and their care. Helping them come to terms with their cancer and their treatment is a vital part of your work.
The role of a clinical oncologist is highly collaborative. You’ll work closely with your patients but also your colleagues as part of a multidisciplinary team. So, you’ll need first-class people skills.
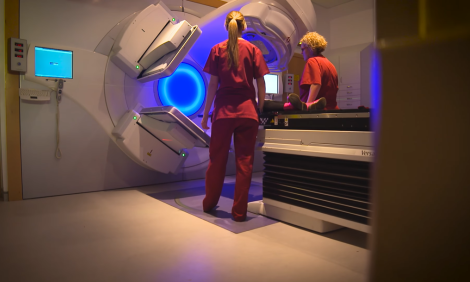
A significant part of your time will be spent in the radiotherapy department. Working alongside colleagues, you’ll be expected to produce personalised treatment plans for all patients, which are a very important part of a clinical oncologist’s work. Technological advances are developing all the time leading to improved patient care and treatment outcomes.
Clinical oncologist is a demanding role, but your skills and expertise will make an enormous difference to your patients and it’s a very rewarding career.
How much can I earn?
You’ll first earn a salary when you start your foundation training after medical school. Find out details of current salary ranges for foundation and specialty training, SAS doctors and consultants on the 'Pay for doctors' page.
How about the benefits?
- make a difference
- flexible and part-time working
- high income early in your career
- work anywhere in the world
- excellent pension scheme
- good holiday entitlement
- NHS discounts in shops and restaurants
Must-have skills
- excellent communication skills to manage a wide range of relationships with colleagues, and patients and their families
- emotional resilience, a calm temperament and the ability to work well under pressure
- teamwork and the capacity to lead multidisciplinary teams
- problem-solving and diagnostic skills
- outstanding organisational ability and effective decision-making skills
- first-class time and resource management for the benefit of patients
Entry requirements
Your first step is medical school. Typically, you’ll need excellent GCSEs and three A or A* passes at A level including chemistry for a five-year undergraduate degree in medicine. Many medical schools also ask for biology and others may require maths or physics.
If you already have a degree, you could study for a four-year postgraduate degree in medicine.
You’ll need to pass an interview and admissions test. You’ll be asked to show how you demonstrate the NHS values such as compassion and respect.
Some medical schools look to recruit a mix of students from different backgrounds and geographical areas, so your educational and economic background and family circumstances could be considered as part of your application.
What are my chances of starting a career as a clinical oncologist?
In 2020, there were 170 applications for 49 places on specialty training for clinical oncology.
How to become a clinical oncologist
After medical school, you’ll join the paid two-year foundation programme where you’ll work in six placements in different settings.
After your foundation programme, you can apply for paid specialty training to become a clinical oncologist, which will take a minimum of seven years.
You may be able to train part time, for example for health reasons or if you have family or caring responsibilities.
Where a career as a clinical oncologist can take you
You could:
- specialise or conduct research in specific cancers
- teach medical students or postgraduate students in training
- get involved in research at universities, the NHS or private sector
-
Consultant Medical Oncologist
Lancaster, LA1 4RP
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- University Hospitals of Morecambe Bay NHS Trust
-
Consultant Clinical Oncologist
Preston, PR2 9HT
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- Lancashire Teaching Hospitals NHS Foundation Trust
-
Consultant Gynaecological Oncologist
Bath, BA1 3NG
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- Royal United Hospitals Bath NHS Foundation Trust
-
Consultant Gynaecological Oncologist Surgeon
London, W12 0HS
- Salary :
- Negotiable
- Type :
- Locum
- Employer :
- Imperial College Healthcare NHS Trust
-
Locum Consultant Gynae-oncologist
Stoke-on-Trent, ST4 6QG
- Salary :
- £109725.00 to £145478.00
- Type :
- Fixed-Term
- Employer :
- University Hospital of North Midlands NHS Trust
-
Locum Consultant Gynaecological Oncologist
Westcliff on Sea, SS0 0RY
- Salary :
- £109725.00 to £145478.00
- Type :
- Fixed-Term
- Employer :
- Mid and South Essex NHS Foundation Trust
-
Locum Consultant Gynaecology Oncologist
Leicester, LE5 4PW
- Salary :
- £105504.00 to £139882.00
- Type :
- Locum
- Employer :
- University Hospitals of Leicester NHS Trust
-
Consultant Clinical Oncologist - Breast
Brighton, BN2 5BE
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- University Hospitals Sussex NHS Foundation Trust (279)
-
Locum consultant Paediatric Haematologist/Oncologist
Nottingham, NG7 2UH
- Salary :
- £109725.00 to £145478.00
- Type :
- Fixed-Term
- Employer :
- Nottingham University Hospitals NHS Trusts
-
Locum Consultant Medical Oncologist – Breast Cancers
London, EC1A 7BE
- Salary :
- £109725.00 to £145478.00
- Type :
- Fixed-Term
- Employer :
- Barts Health NHS Trust
-
Consultant Medical Oncologist (Gastrointestinal & HPB Cancers)
Southampton, SO16 6YD
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- University Hospital Southampton NHS Trust
-
Substantive Consultant Medical Oncologist (Gastrointestinal cancer)
london, NW3 2QG
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- Royal Free London NHS Foundation Trust
-
Consultant Medical Uro - Oncologist (Germ Cell/Prostate/Bladder)
Brighton, BN2 5BE
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- University Hospitals Sussex NHS Foundation Trust (279)
-
Fixed Term (12 months) Consultant Clinical Oncologist - Breast
Brighton, BN2 5BE
- Salary :
- £105504.00 to £139882.00
- Type :
- Fixed-Term
- Employer :
- University Hospitals Sussex NHS Foundation Trust (279)
-
Consultant Clinical Oncologist - Urology and Colorectal tumour sites
Derby, DE22 3NE
- Salary :
- £105504.00 to £139882.00
- Type :
- Permanent
- Employer :
- University Hospitals of Derby and Burton NHS Foundation Trust
-
Locum Consultant Paediatric Oncologist with special interest sarcoma
London, NW1 2BU
- Salary :
- £109725.00 to £145478.00
- Type :
- Fixed-Term
- Employer :
- University College London Hospitals NHS Foundation Trust
-
Consultant Clinical Oncologist (Upper GI,HPB and Lung Cancer)
London, NW3 2QG
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- Royal Free London NHS Foundation Trust
-
Consultant Clinical Oncologist with Breast & Lower GI Cancers Interest
Coventry, CV2 2DX
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- University Hospitals Coventry and Warwickshire NHS Trust
-
Consultant Medical Oncologist with an interest in Breast AO & Lung
Eastbourne, BN21 2UD
- Salary :
- £109725.00 to £145478.00
- Type :
- Permanent
- Employer :
- University Hospitals Sussex NHS Foundation Trust (279)
Showing 6 of 19 results
-
See the Royal College of Radiologists website for further information about being a clinical oncologist and stories from doctors working in clinical oncology.